Why do we need a One health approach?
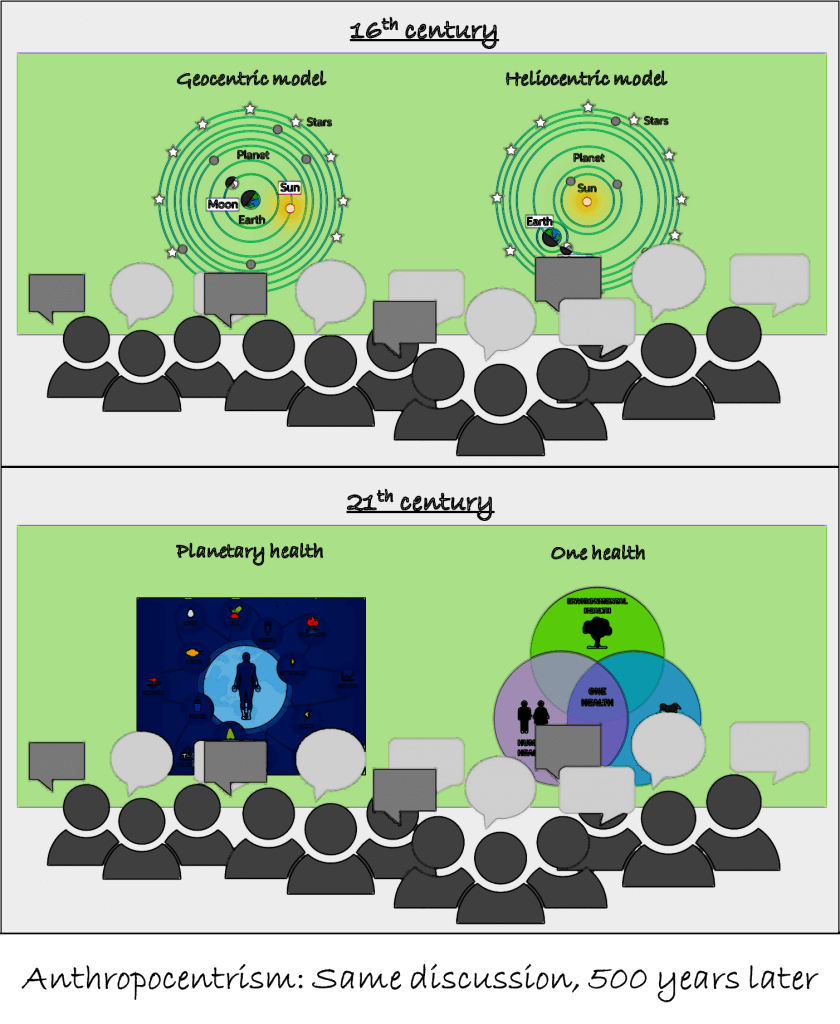
The last one and a half years have drastically shown how vulnerable mankind is on earth. The Covid-19 pandemic has revealed the many problems we face today but also in the future. Since Covid-19 disease originates from zoonotic coronavirus, there is a strong linkage between humans, animals, and the environment. Experts suggest that the 2019 pandemic outbreak was not the last one to come [1]. In order to tackle the problem and to be prepared for the future an integrated perspective is required. This is where the One Health approach comes into play.
Author: Benedikt Wittmann (GCE 2019)
What is the One Health approach?
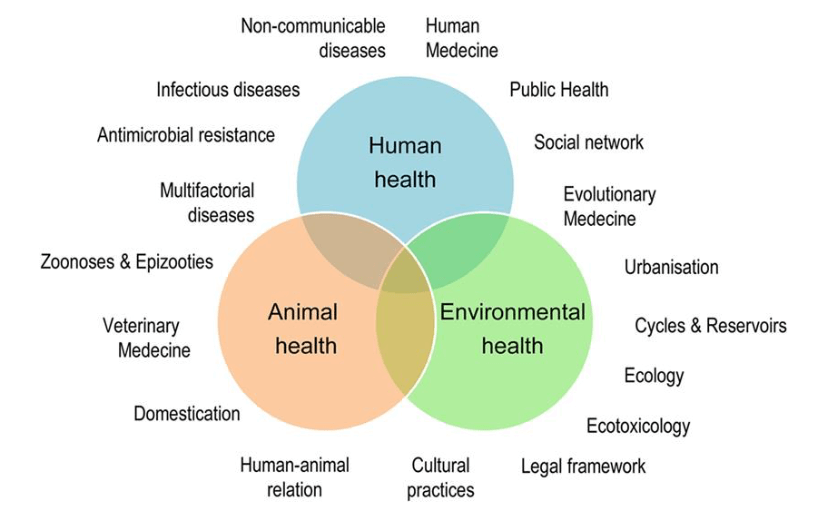
Created in 2005, the One Health concept incorporates a multisector expertise and follows a holistic and transdisciplinary approach [2]. Generally speaking, health refers to the wellbeing of the physical, mental, and social status. But because the health issues are broad and complex, the One Health approach primarily focuses on health crisis related to ecological and environmental drivers and underscores the interconnectedness of health between humans, animals, plants, and the environment where they inhabit. It holds that to achieve ultimate human health, animals, plants, and environmental health needs to be addressed as well. Health threats shared by people, animals and the environment including zoonotic diseases, antimicrobial resistance, food safety and food security, vector-borne diseases, and environmental contamination are all common One Health issues [3].
Example of One Health – Antimicrobial Resistance
One example of applying the One Health approach in combating global health crisis is addressing antimicrobial resistance (AMR). In order to protect humans, livestock and agricultural production from bacterial infection, drugs containing antibiotics and antimicrobial agents have been widely used across the world. However, the pervading use of antimicrobial drugs has given rise to the microorganisms’ capability to adapt to those drugs. Consequently, the antimicrobial-resistant bacteria continue to harm human and animal health. What is worse, the antibiotics provide opportunities for zoonotic bacteria to develop resistance genes while transmitting to human bodies via food sources (e.g. meat products), direct animal contact, and contaminated environmental sources [4]. Facing the rapidly increasing threat posed by AMR, transdisciplinary collaboration and intersectoral countermeasures must come into force, such as the One Health approach.
Following this transdisciplinary approach, several organizations raise awareness of AMR. For instance, the World Health Organization developed the Global Antimicrobial Resistance Surveillance System (GLASS), which drives local, national, and regional action. Laying the main focus on the collection, analysing and sharing of AMR data on global level, decision making on different levels should get enhanced [4,5].
According to the latest report, 109 countries and territories worldwide have enrolled in the Surveillance System until May 2021. The Assessment shows that GLASS significantly helped to foster the development of national AMR surveillance systems. As next steps it is aimed to enhance the completeness and quality of data [6].
Outlook
Most likely the Covid-19 pandemic has not been the last zoonotic disease posing a threat to humans. Close collaboration of different domains will be a key contribution for solving and preventing further crisis. The One Health Approach seems therefore a good possibility to tackle health related challenges in the future. Especially the holistic approach entails many opportunities for solutions on the global, national and local level. However more applicable frameworks should be provided, in order to enable a better implementation by different stakeholders with varied interests and interpretations of the One Health approach. Effective performance of One Health initiatives at all levels could hardly be achieved without developing more coherent and endurable frameworks for the increasingly diversified practitioners.
References
[1] Zowalaty, M. E., & Järhult, J. D. (2020). From SARS to COVID-19: A previously unknown SARS- related coronavirus (SARS-CoV-2) of pandemic potential infecting humans – Call for a One Health approach. One Health, 9, 100124. doi: 10.1016/j.onehlt.2020.100124
[2] Destoumieux-Garzón, D., Mavingui P, Boetsch G, Boissier J, Darriet F, Duboz P, Fritsch C, Giraudoux P, Le Roux F, Morand S, Paillard C, Pontier D, Sueur C and Voituron Y (2018). The One Health Concept: 10 Years Old and a Long Road Ahead. Front. Vet. Sci. 5:14. doi: 10.3389/fvets.2018.00014
[3] Centers for Disease Control and Prevention (2018). National Center for Emerging and Zoonotic Infectious Diseases. One Health Basics. Last viewed 23.07.2021 from https://www.cdc.gov/onehealth/basics/index.html
[4] Schneider, M. C., Munoz-Zanzi, C., Min, K and Aldighieri, S. (2019). “One Health” From Concept to Application in the Global World. Global Public Health. doi: 10.1093/acrefore/9780190632366.013.29
[5] WHO (2021). Global Antimicrobial Resistance and Use Surveillance System (GLASS). Last viewed 27.07.2021 from https://www.who.int/initiatives/glass
[6] Global antimicrobial resistance and use surveillance system (GLASS) report 2021. Geneva: World Health Organization; 2021. Licence: CC BY-NC-SA 3.0 IGO.